Redesigning Health(care)
Shani Abass
→BFA GD 2021
For the last few years, I’ve been saying that I want to be a healthcare designer or that I want to go into healthcare technology, and I’ve always explained that as the practice of designing products to help people with conditions such as cancer, dementia, strokes, and depression. Throughout my degree, I have tried to address these issues by developing mental health chatbots, therapeutic virtual reality experiences, and wearable monitoring devices—tools that would help alleviate the symptoms of diagnosed mental and physical illnesses.
Over the past few months, I’ve started to think deeply about my own health. As I’ve been largely stuck indoors, I’ve gained a few pounds, lost a lot of muscle tone, done a lot less cardio, eaten a lot more junk food, and absorbed significantly less vitamin D than usual. Overall, I’m a lot less healthy. However, I’ve still been full of energy, well-rested, and generally feeling well. This is because, although I haven’t been eating healthily or exercising, I have years of immunity built up through the provision of good food, shelter, a safe neighborhood to go for walks in, health insurance, access to gyms, and reduced stress due to financial security. I can therefore afford to be a bit unhealthy for a few months.
I have also considered my health in relation to the virus, and how I have a relatively low risk of contracting it. This is because I can live in isolation with my parents and do not have to frequently encounter other members of the community. My parents have jobs that allow them to work from home, I have a backyard I can exercise in, and I have internet access which allows me to take my classes online, order all of my groceries, and access entertainment. All of these factors significantly reduce my risk of exposure to the virus. I’ve realized that although there are lifestyle changes that can be made and treatments that can be administered, ultimately, the risk of contracting diseases and being severely affected by them largely boils down to socially determined risk factors that need to be addressed preventatively rather than therapeutically.
A topic of contention in the UK at the moment is whether or not the government should continue to provide free school meals during school vacations to children who, as a result of pandemic-induced financial crises, cannot afford to eat. At the same time, the government has proposed calories be on food packaging in an effort to reduce obesity. However, as many people have pointed out on social media, the socioeconomic system simply does not allow poorer people to eat healthily. It is not just about buying inexpensive fruits and vegetables, it is about having a fridge to store them in, and a stove, oven, or microwave to cook them with, as well as gas, electricity, kitchen utensils, crockery, and cutlery. For some families, it is most practical to eat things like potato chips every day as they are inexpensive, filling, and do not require additional resources to prepare them. Indeed, eating like this does negatively affect one’s health; it can lead to nutrient deficiencies, obesity, and low immunity overall, which are significant risk factors during a pandemic.
Various news stories and events have also highlighted the fact that mental health issues are also widespread among less affluent communities. In addition to those with financial struggles experiencing daily stress and anxiety, many people with pre-existing mental health conditions do not receive adequate help due to a lack of funding. Furthermore, members of marginalized groups such as ethnic minorities and LGBTQ+ people are often discriminated against in the healthcare system; for instance, the National Transgender Discrimination Survey Report on Health and Health Care by Grant et al. found that 19% of respondents had been refused care as they were transgender, with most of these respondents being people of color, and 28% had postponed treatment due to negative experiences with discrimination.1 The discrimination they face in their day-to-day lives also negatively affects their physical health. For example, a 2016 study conducted by Leitner et al. found that Black people were more likely to die from circulatory disease in counties with higher levels of racial bias.2
As I look to pursue a career in healthcare design, I intend to create tools that minimize socially determined risk factors in addition to the standard symptom tracking, reporting, and diagnosing apps. We need to start with data visualizations explaining how and why tax money must be redistributed, products that allow for the inexpensive storage and preparation of nutritious meals, and experiences that create empathy for people in different marginalized groups to reduce systemic discrimination.
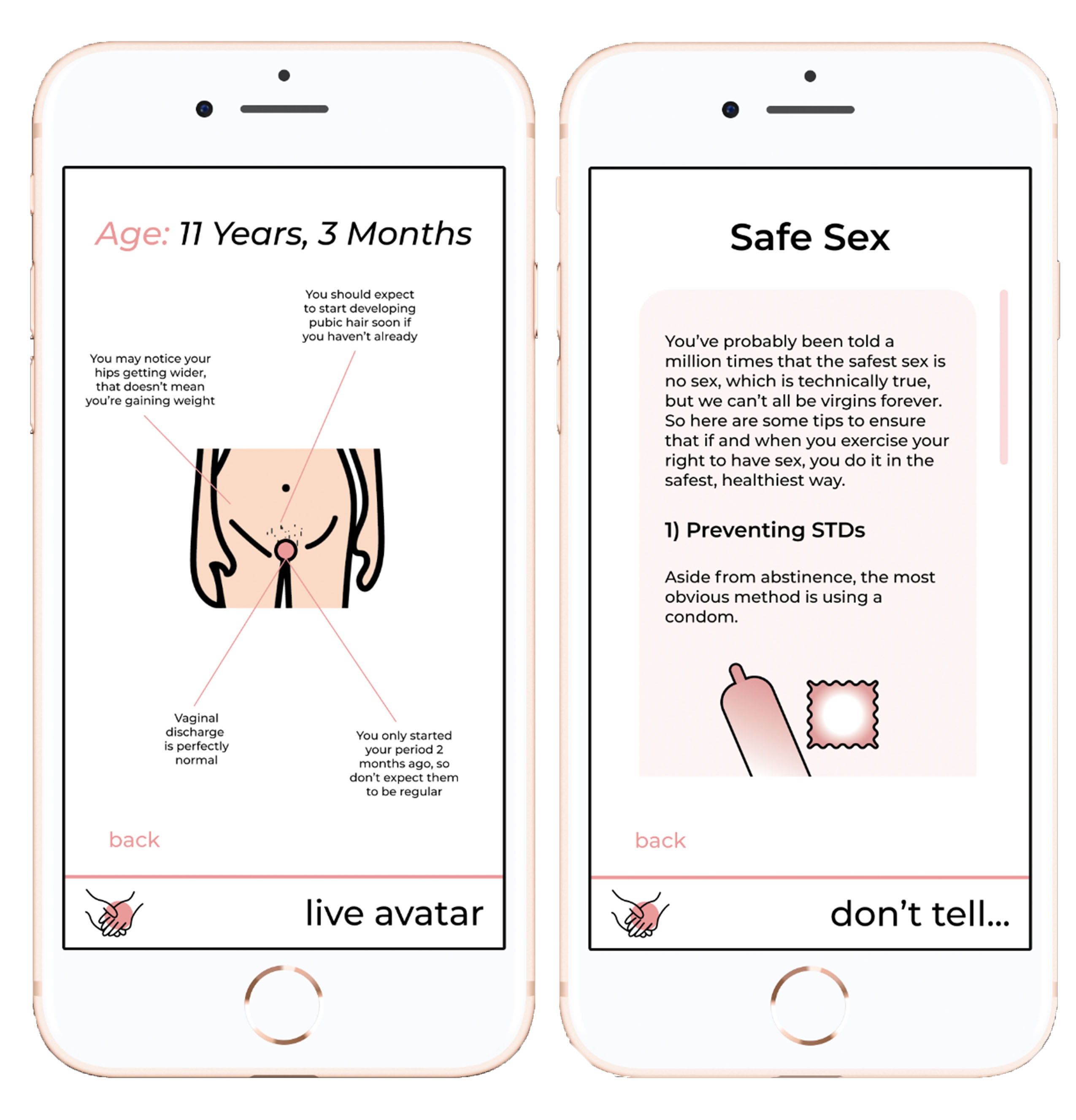 Pages from the author’s “TheGirlGuide” app.f
Pages from the author’s “TheGirlGuide” app.fOne systemic issue that I’ve addressed in my own work is sex education. In my sophomore year, I developed a prototype for an app called “TheGirlGuide.’ It was influenced by readings and discussions during a Wintersession liberal called “Race, Class, and Girlhood,” during which I discovered how much disparity there was in sex education for girls both across the world and among my classmates. This disparity was due to multiple factors from a lack of resources in schools to cultural beliefs at home. One issue that emerged was the prevalence of unsafe sex and illnesses resulting from girls’ lack of knowledge and embarrassment about asking questions. My app therefore provides young girls with real-time information on how their body is changing as they go through puberty, as well as age-appropriate resources and tips for related issues such as sex and relationships, mental and physical health, and drugs and alcohol, and an anonymous support group. By educating young people about these issues early on and allowing them to make more informed choices, I hope that more serious medical issues will be prevented down the line.
Another key issue that needs to be addressed is the delivery of, and access to, healthcare itself. In addition to economic factors such as access to health insurance, and social factors such as racial and LGBTQ+ discrimination, we face barriers such as geographical and digital access. While telehealth is a great way to reduce paid hospital visits and allow people to access healthcare from remote areas, it is also not accessible to people without access to the internet or even a sophisticated digital device. Interventions such as funded monthly clinics and care packages (containing items such as illness-prevention guides, first-aid items, vitamins, and general wellbeing tips) in areas where telehealth is not a viable solution could also be beneficial.
In conclusion, a redefinition of “health” as a multidimensional combination of socioeconomic factors allows us to redesign “health(care)” and move away from the current conception of it as purely clinical treatment. Redesigning health(care) can’t start with treating symptoms; that’s already too late. It needs to start with redesigning society, which is a much bigger challenge that involves the undoing of systemic discrimination in multiple areas. But it’s a challenge we must take on if we want healthcare devices to have a real impact on a wide range of users.
1 Grant, J.M., Mottet, L.A., Tanis, J., Herman, J.L., Harrison, J., Keisling, M. (2010). National transgender discrimination survey report on health and healthcare. Washington (DC): National Center for Transgender Equality and National Gay and Lesbian Task Force,1–23. https://cancer-network.org/wp-content/uploads/2017/02/National_Transgender_Discrimination_Survey_Report_on_health_and_health_care.pdf
2 Leitner, J. B., Hehman, E., Ayduk, O., & Mendoza-Denton, R. (2016). Blacks’ death rate due to circulatory diseases is positively related to whites’ explicit racial bias: A nationwide investigation using project implicit. Psychological Science, 27(10), 1299–1311. https://doi.org/10.1177/0956797616658450
Shani Abass is an aspiring UX designer currently studying remotely from her home city of London. She just couldn’t survive four years of colleege without a real cup of tea.